Abstract
Background: Recent studies with CPX-351 indicate that a fixed 5:1 molar ratio of Cytarabine to Daunorubicin is the most synergistic in pre-clinical models and the most efficacious in patients. This molar ratio of two standard of care drugs in Acute Myeloid Leukemia (AML) is preserved via liposomal encapsulation. A 5:1 ratio has superior clinical benefit to non-encapsulated combinatorial drug delivery. Conceptually, we have created the same framework by designing an in vitro screen to indicate the optimal ratio of two standard of care AML drugs, 5-Azacitidine (5-Aza) and Venetoclax. We have chosen this two-drug combination for its efficacy in the relapsed setting, and its tolerable safety profile which makes it amenable to patients with a high cumulative anthracycline exposure or scenarios where more intensive regimens cannot be tolerated. An iterative synergy screen was performed to probe for pathways that are co-opted by AML cells to evade and resist 5-Aza and Venetoclax combination therapy.
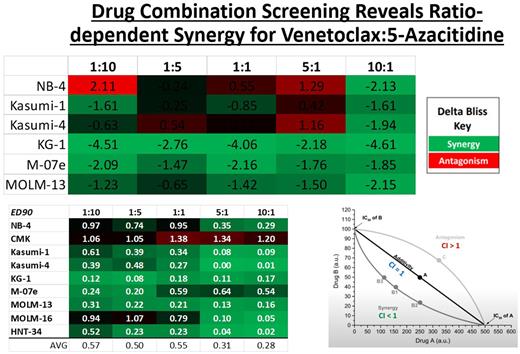
Methods: A high throughput combination screen generated over 100,000 wells of data across 9 cell lines, representing 7 of the French-American-British (FAB) subtypes, and 5 of the World Health Organization (WHO) genetic subtypes of AML. The Combination Index (CI) method with the software Calcusyn and the Delta Bliss model were used to evaluate in vitro synergy potential. Molar ratios of 5-Aza:Venetoclax evaluated were: 1:10 , 1:5 , 1:1 , 5:1 , and 10:1. A panel of 112 drugs was screened which includes all FDA approvals since 2015, drugs which are routinely used in AML treatment, and several new therapies which are in Phase I/II trials. This 112-drug panel was used to pharmacologically probe for pathways of resistance to 5-Aza and Venetoclax combination therapy.
Results: Patterns of antagonism and synergy across different genetic and phenotypic backgrounds were observed, but on average a fixed molar ratio of 1:10 5-Aza:Venetoclax was the most synergistic. Of the 112 drugs used to probe for resistance mechanisms to 5-Aza/Venetoclax combination therapy, MCL-1 Inhibitors emerged as the most promising.
Conclusion: Our data demonstrates that a hypomethylating low dose, not a high cytotoxic dose of 5-Aza, combined with Venetoclax at a ratio of 1:10 may have potential for liposomal encapsulation to preserve optimal cell killing ability. Additionally, pathways of resistance to a standard of care regimen were uncovered which reveal the importance of MCL-1 in resistance to 5-Aza/Venetoclax therapy, and to a lesser extent BCL-XL. This puts forth the idea that a small molecule targeting BCL-2 and MCL-1, while avoiding targeting BCL-XL which causes a dose-limiting thrombocytopenia, may be a rational strategy for overcoming resistance to BCL-2 directed therapy.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal